Christian Doppler Laboratory Modules
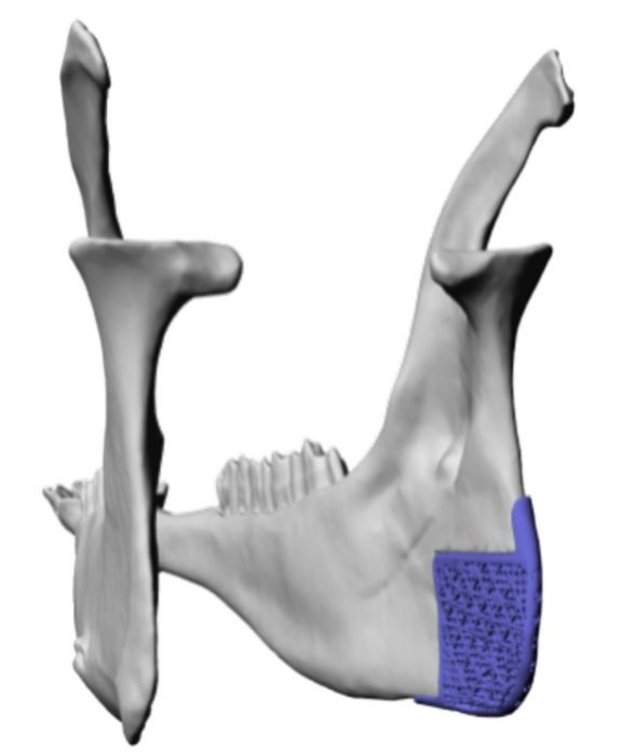
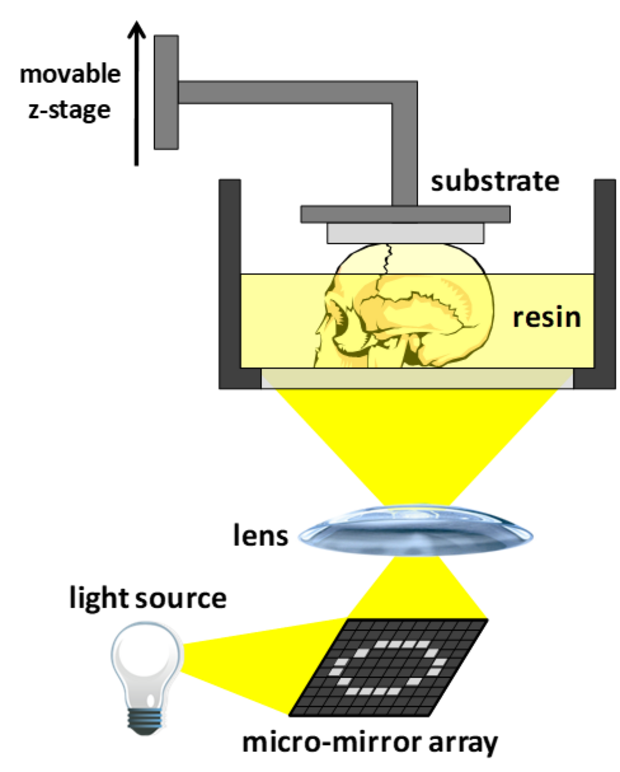
The combination of biomaterials as basis for regenerative medicine with 3D printing has gained a lot of attention in the last decade. The ability to provide patient-specific biocompatible implants, which support the self-healing capacity of the human body is very appealing. In case of bone regeneration, especially in the oral and maxillofacial region, the advantages of this combination are obvious. Bones possess structural features, arrangements of dense as well as highly porous elements, which can perfectly be mimicked by 3D printing processes. Especially lithography-based additive manufacturing techniques (L-AMTs, i.e., photopolymer-based 3D printing) have been found to be ideal technologies to generate bone regeneration constructs, mainly owing to their optimal feature resolution (ideal for cell attachment), their reasonable production times, and their possibility to provide highly filled bone-mineral (bio)composites or -ceramics.
Biocomposites are obtained by the photopolymerization of formulations filled with, e.g. hydroxyapatite or tricalcium phosphate; a subsequent debinding and sintering process leads to dense ceramics. However, a lot of problems arise from the material side. First of all, the photopolymerization of highly filled formulations is critical as curing depths are low owing reflection and scattering of light. Insufficient mechanical properties of the photopolymer matrix and shrinkage stress, furthermore, lead to unsatisfactory final properties of the materials or even failure. While the biocompatibility of the photopolymer matrix for binder removal and sintering is irrelevant, it plays a central role in biocomposites. The biocompatibility of commonly used (meth)acrylates as precursors is limited, moreover their unfavorable degradation behavior (bulk degradation), and highly immobile degradation products, like (poly(meth)acrylic acid), are very problematic. Most of these problems could be solved by establishing vinyl esters as alternative reactive groups in precursor formulations for bone constructs, however, a lot of fundamental questions arose from this decision as this class of monomeric precursors is not established in the coating industry, which is the main resource for base formulations and additives for classical (meth)acrylate based photopolymer precursors for L-AMTs.
Module 1: Chemistry of Biomaterials and Polymerization
Solving the issues concerning the low light penetration, the mechanical properties as well as biocompatibility and -degradability will be the central task of Module 1 of the CD laboratory. In order to improve the vascularization of the implants (dense ceramics or biocomposites), a “biologization” concept will be pursued by addition of a biological matrix that supplies nutrients and (growth) factors. By modification of extracted extracellular matrix (ECM), e.g. human placenta ECM, a bio-ink will be developed, which is filled into the porosity of the 3D printed bone substitute.
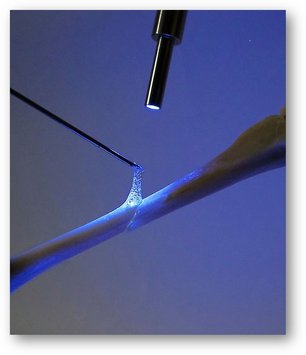
Bone adhesives were found to be a clinically desired product for the fixation of the 3D printed patient-specific bone graft substitute at the bone defect during oral and maxillofacial surgery. Fixation with plates and screws is critical as stress peaks in the material or bone may lead to cracks and failure of the implantation. Here, we exploit the knowledge gained within this Module and transfer the biocompatible formulations to in situ cured materials. This project raises another set of questions, most importantly the bone adhesivity as well as the introduction of porosity as demanded for tissue regeneration.
Within this Module, the biomedical examination of components as wells as final constructs is performed to obtain important feed-back for the fundamental material studies.
Modul 2: Advanced Systems for 3D Printing
The 3D printing process itself is very complex and stresses further considerations. On the one hand the layer-wise principle of manufacturing of L-AMTs was found to be very favorable for cell attachment and growth of tissue, on the other hand, however, holds critical disadvantages for the quality of the final parts as delamination, boundary effects, and layer inhomogeneity often lead to material failures in 3D printed constructs, esp. in highly filled systems.
Solving these issues is covered in Module 2 of the CD laboratory. Here, the measures from Module 1 to improve the material properties, specifically photoreactivity, curing depths and shrinkage stress reduction during layer-wise curing process are examined by the investigation of 3D printed parts. Moreover, instrumental measures to improve the layer quality by considering a new 3D process will be investigated.




baudisLAB • Institute of Applied Synthetic Chemistry • Getreidemarkt 9/163, 1060 Vienna, Austria • stefan.baudis@tuwien.ac.at


